Population Health

Drug use in the elderly
In Population Health
Bookmark
Record learning outcomes
Much closer working between health professionals and more integrated interventions are essential to tackle inappropriate prescribing and poor adherence in elderly patients
Most elderly people have health issues. In a 2018 report, Use of Medicines by the Elderly: the Role of Pharmacy in Promoting Adherence, the International Pharmaceutical Federation (FIP) notes that sensory and cognitive impairment, as well as musculoskeletal, co-ordination and balance problems, are common in elderly people and all can contribute to non-adherence. So how can pharmacists help tackle this pressing problem?
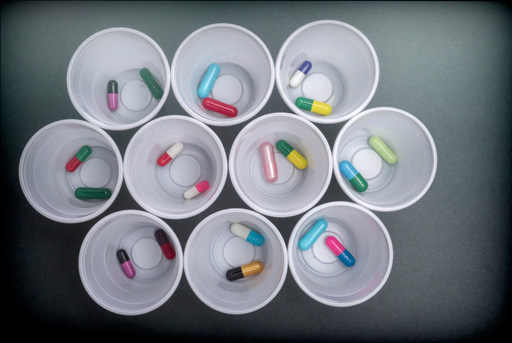
Perils of polypharmacy
In 2016, a woman and man aged 65 years could expect to live another 20.9 and 18.6 years respectively but, for more than 40 per cent of this time (9.7 and 8.2 years respectively), the person will not be in good health, says the Office for National Statistics (ONS). The Health Survey for England, for instance, found that in 2016, 29 per cent of those aged 60-64 years suffered from at least two chronic conditions, rising to almost half of those aged 75 years and older.
This burden of illness among the elderly inevitably drives polypharmacy. Researchers from Cork University Hospital recently studied 410 people aged at least 65 years who were hospitalised during their last year of life. Their mean age was 80.8 years and 63.7 per cent were severely frail. During the last year of life, patients spent a median of 32 days in hospital and received a mean of 23.8 medicines during all their admissions, with 43.6 and 17.3 per cent receiving at least 25 and 35 medications respectively.1
While an admission can address the immediate clinical problem, hospitalisation can take its toll, impairing physiology, depleting the body’s reserves and reducing resistance. This makes the time immediately after discharge a particularly “fragile period”2, with an increased risk of complications and readmissions. Yet actions requested in hospital discharge summaries are often not enacted.
In one study3, a GP reviewed the records of 300 people aged 75 years and older from 10 general practices in England who were discharged after an emergency admission. While the reviewer did not consider documented occasions where the GP disagreed with the discharge summary to be failures, the study found that the primary care team failed to process requests in 46 per cent of cases.
Seventeen per cent of the requested medication changes were not made, 26 per cent of the tests were not completed and follow-up was not arranged in 27 per cent of cases. The study suggested 8 per cent of these failures potentially caused harm.
Our ageing population
Epidemiologists have warned for years that the UK population is steadily ageing. According to the Office for National Statistics (ONS), 11.8 million UK residents were aged 65 years and older in 2016. That’s almost one in six (18 per cent) of the total population and compares with 9.1 million in 1991.
By 2066, the ONS estimates 20.4 million people will be aged 65 years and older, when they will account for more than a quarter (26 per cent) of the UK population.
The number of people aged 85 years and older will show the fastest increase. In 2016, 1.6 million people (one in 50 of the population) were aged 85 years and older, while, in 2017, almost 580,000 people were 90 years of age and older and 14,430 were centenarians.
In 2002, by way of comparison, 7,800 people were centenarians. By 2041, the ONS estimates that 3.2 million people will be aged 85 years and older, rising to 5.1 million in 2066. In contrast, the ONS projects that the population aged 16-64 years will increase by just 2 per cent by 2041 and 5 per cent by 2066.
Inappropriate prescribing
There is little doubt that over-medicating is common. During the last year of their life, the Cork study found that 81.5 per cent of patients were prescribed at least one potentially inappropriate medication (PIM) at discharge and 34.0 per cent received at least three PIMs. Lipid-lowering drugs, proton pump inhibitors, antipsychotic agents and calcium supplements accounted for 59 per cent of PIMs.1
Fully implementing the STOPPFrail recommendations – a list of 27 indicators to assist deprescribing in frail older people with poor one-year survival prognosis – would have resulted in the discontinuation of 23 per cent of the long-term medications.1
Another recent study from Ireland examined the records of 38,229 patients aged 65 years and older from 44 general practices between 2012 and 2015. Each year, between 10.4 and 15.0 per cent of the patients were admitted to hospital. The rate of potentially inappropriate prescribing (defined using the STOPP2 criteria) varied from 45.3 to 51.0 per cent, depending on the year.
After adjusting for confounders, potentially inappropriate prescribing increased the risk of hospitalisation by 24 per cent, yet patients admitted to hospital were 72 per cent more likely to show potentially inappropriate prescribing after discharge compared to before admission. Several reasons might account for this including intensification of existing regimens and failing to stop drugs or reduce doses in the community.4
PIMs seem to be associated with worse economic and clinical outcomes. A study from Finland followed 10,333 people aged 65 years or older and the same number of matched controls for 12 years. The risk of death was 38 per cent higher for one month of exposure to a PIM during this time, rising to a 67 and 81 per cent increased risk after three and six months of use.
The risk of hospitalisation following a fracture was 20 per cent higher after one month of exposure to a PIM and 30 per cent higher after three and six months’ exposure.
The mean number of hospital episodes (e.g. admissions and follow-up appointments) was higher in people taking PIMs compared with controls (33.9 and 22.4 respectively). Hospital costs were 15 per cent higher in people taking PIMs compared with hospitalised controls, but 50 per cent greater when the analysis included people who were not admitted during the 12-year follow-up.5
The FIP report, Use of Medicines by the Elderly, notes that medication reviews offer a “powerful approach to the resolution of polypharmacy” and are “demonstrably effective”. For instance, a Swedish study6 analysed 1,720 people aged 75 years or older who underwent a medications review in primary care.
Patients received a mean of 11.3 drugs, ranging from one to 35, and 84 per cent experienced at least one drug-related problem, such as unnecessary medications (39 per cent), excessively high dose (21 per cent) and incorrect drugs (20 per cent). PIMs accounted for 12 per cent of the drug-related problems.
A medication review significantly reduced the number of people taking at least one PIM (from 29.7 to 17.4 per cent) and those using at least three psychotropic drugs (from 23.0 to 17.2 per cent). Withdrawing drugs (47 per cent), reducing dose (21 per cent) and changing medication (9 per cent) emerged as the commonest suggestions from pharmacists to GPs following the review.6
Nevertheless, medication reviews, especially those performed in the patient’s home or care home, can be time-consuming. Remuneration for pharmacists, the FIP report notes, can be “cumbersome or inadequate”. The most effective reviews depend on a good working relationship with the prescriber, while obtaining consent from cognitively impaired patients can be challenging. “Nevertheless, when these logistical problems can be overcome, medication reviews provide a very good mechanism for managing polypharmacy,” the report comments.

Improving adherence
Medication reviews also offer a valuable mechanism to improve adherence, especially as older people can have several problems that could make compliance a particular problem, the FIP report notes. Cognitive impairment, for example, can result in inappropriate decision-making about medicines and forgetfulness. Musculoskeletal problems can undermine a person’s manual dexterity, making the handling of tablets, capsules and packaging difficult.
Healthcare professionals may not notice mild or early cognitive decline during the brief encounters typical of many settings, including pharmacy, so the FIP suggests that pharmacists and all other healthcare professionals be trained and supported to detect cognitive decline.
Meanwhile, a report published in January 2018 by the All-Party Parliamentary Group on Hunger found that in 2011, 1.3 million older people were malnourished or at risk of malnutrition. The report commented that malnutrition in older people “is often intertwined with loneliness and social isolation”.
Against this background, the FIP report suggests that pharmacists should assess the health literacy of patients and carers, then guide the discussion and enhance understanding so that they can engage in decision-making.
Pharmacists can also “dispel any ill-founded concepts that might lead to intentional non-adherence” and “make it as easy as possible for older patients to take their medicines correctly” by, for example, keeping medication regimens as simple as possible and reviewing them regularly.
Dose administration aids can help patients and carers use the “right medicine in the right dose at the right time” and keep track of adherence. Pharmacists can also support family members to help patients adhere and provide reminders to, for example, fill repeat prescriptions.
The FIP report notes, however, that none of these interventions is self-sustaining, therefore pharmacists should:
- Reiterate the messages opportunistically (e.g. when scripts are being refilled)
- “Repeatedly” ask if any medicine is causing problems
- Address any issues (ideally in consultation with the prescriber)
Pharmacists should also observe the administration of certain drugs (e.g. inhaler technique) regularly. Other research (which the current author contributed to) suggests that pharmacists should ask about difficulties swallowing medicines,7 food and drink.
Use of Medicines by the Elderly notes, however, that community pharmacists are often relatively isolated from other healthcare professionals. “This isolation... limits the scope of interventions that could improve adherence if health professionals were able to work together in a more integrated way,” the report argues.
Such interventions include improving communication between primary and secondary care, closer monitoring of patients and improved self-management.4 Medication reviews are also an important element, especially for elderly people, and new protocols and guidelines are being developed to facilitate deprescribing (see deprescribing.org).4
One thing seems certain – multidisciplinary working across traditional boundaries is essential to drive improvements. And that could put community pharmacists at centre stage.
A prescription for social isolation?
Studies suggest that between 2 and 16 per cent of people aged 65 years and older report severe loneliness. At any time, up to 32 per cent of people older than 55 years of age feel lonely.8 According to the Government, three-quarters of GPs report seeing between one and five people a day suffering with loneliness, which is linked to, among other ailments, heart disease, strokes and Alzheimer’s disease.
In October, the Prime Minister announced that by 2023 GPs in England will be able to refer patients experiencing loneliness to community activities and voluntary services – so-called ‘social prescribing’ (see PM's recent article on the topic). Local interventions suggest social prescribing could work. Ageing Better in Camden (ABC), for example, is a programme that aims to address social isolation and loneliness in people over 60 years.
An evaluation of eight projects funded by ABC consistently reported:
• Reduced social isolation and increased wellbeing
• Increased confidence and independence
• Stronger relationships across communities and generations.
The projects use a variety of recruitment methods, although engaging the most socially isolated older people still proves difficult. In October 2015, for example, ABC started a two-year project that commissioned 13 pharmacies to identify older people who were lonely or isolated and refer them to a ‘community connector’, who discusses their interests and suggests activities.
ABC admits that “the project experienced a slow start with only 25 referrals” in the first year. In the second year, ABC introduced a scratch card that helped pharmacies to “allow older people to walk through the referral process themselves, self-selecting what local activities and community initiatives interested them”. The card reflected feedback that people were reluctant to discuss personal issues in a busy pharmacy.
Any further collaborations with pharmacies need to “be mindful that a ‘one size fits all approach’ does not work due to different management styles, and available time, space and staff in individual pharmacies”, ABC says. Nevertheless, the “project showed that pharmacies play an important role as social connectors at a community level with local groups and centres”.
Further information
• Ageing Better in Camden
References
- Age and Ageing 2018; 47:749-753
- BMJ Open 2017; 7:e018443-e018443
- British Journal of General Practice 2018; 68:e576-e585
- BMJ 2018; 363:k4524
- The European Journal of Health Economics 2018; DOI:10.1007/s10198- 018-0992-0
- BMC Health Services Research 2018; 18:616
- Pharmacy in Practice 2005; 15:411-414
- Journal of the Royal Society of Medicine 2012; 105:518-522

