OTC

The obesity agenda
In OTC
Bookmark
Record learning outcomes
With obesity on the rise, the Welsh Government has published a new strategy to help people manage their weight and there are plenty of ideas to help people all across the UK
Obesity is moving up the agenda in Wales. The Welsh Government has recently published a new strategy document with the aim of seeing the country as one of the first in the world to witness declining rates of obesity over the next 10 years. In Wales, 1.5 million people, or 59 per cent of the adult population, are overweight or obese, with numbers rising each year. If this trend continues, the number of overweight or obese adults is projected to increase by 160,000 people to 64 per cent of the Welsh population by 2030.

Preventing obesity is a complex but essential challenge, requiring input and commitment from individuals, communities and society as a whole. Evidence shows having a healthy weight is one of the most effective ways to reduce the risk of long-term health conditions, including joint problems; high blood pressure; coronary heart disease; stroke; type 2 diabetes; endometrial, breast and colon cancers; and respiratory problems.
“Obesity is projected to overtake smoking as the nation’s biggest public health challenge,” says Welsh health minister Vaughan Gething. “Too often people are confronted with unhealthy choices and bombarded with messages that promote unhealthy options, a culture that is occurring not just in Wales but across the Western world; we need to redress the balance. Small steps towards healthier habits can create big change, and this is the basis of the strategy. Everybody needs to play a role – prevention cannot be achieved by Government, the NHS or any other individual sector alone.”
Four themes
The Welsh Government’s new Healthy Weight: Healthy Wales strategy document aims to deliver healthy settings and environments to allow people of all ages to make healthy choices. It focuses on the prevention of obesity, encouraging people to eat more healthily and become more active. The plan is broken into four themes:
- Healthy environments: This focuses on changing the way people shop, eat out, travel and use outdoor spaces
- Healthy settings: This includes childcare settings, schools and higher and further education, workplaces and community settings
- Healthy people: This includes providing people with the opportunity to regularly discuss their lifestyle choices with healthcare professionals
- Leadership and enabling change: This intends to drive improved leadership and accountability to deliver Healthy Weight: Healthy Wales across all sectors.
With more than a quarter of Welsh children overweight or obese at reception age, preventing and reducing obesity in children is considered a priority. Dr David Tuthill, the Royal College of Paediatrics and Child Health (RCPCH) officer for Wales, is urging the Welsh Government, the Welsh NHS and all of the other partners to embrace this vital plan and work in partnership with families.
These strategies should not be restricted to Wales, however, as they could be, and are being, incorporated into work within other parts of the UK. In January 2019, secretary of state for health and social care Matt Hancock addressed the All-Party Parliamentary Group (APPG) on Obesity at the International Conference on Obesity. He said that “tackling obesity means tackling social, environmental, physical and psychological pressures, and giving people the capability they need to eat healthily” and is a “shared responsibility for society”.
Obesity is projected to overtake smoking as the nation’s biggest public health challenge
Pharmacy support
Andrew Evans, chief pharmaceutical officer for Wales, believes that pharmacists and pharmacy teams have a key role in promoting healthy lifestyle choices, including providing advice on weight management. He says: “In our Healthy Weight: Healthy Wales strategy, we make a commitment to increasing the confidence and skills of healthcare professionals to help them routinely hold conversations with people about weight sensitively. It also sets out our commitment to delivering tailored campaigns for adults and children providing trustworthy, up-to-date and consistent advice.”
According to the Public Health England (PHE) Adult Obesity: Applying All Our Health document, updated in June 2019, healthcare professionals should “provide information, advice and support around healthy lifestyles and, where appropriate, refer to weight management services as part of routine daily contact with individuals”.
The recommendations for frontline healthcare professionals, such as the pharmacy team, include:
- Speak to patients about achieving and maintaining a healthy weight, referring them to information or services if necessary
- If a patient discusses their weight themselves, acknowledge their concerns and commend them for raising the issue and wanting to take action
- Recognise that individuals may take time to find the right solution for them; achieving and maintaining a healthier weight sometimes takes multiple attempts and there isn’t a single solution that works for everyone
- Understand that a healthier weight is primarily achieved and maintained through improving dietary intake, portion control and being more physically active
- Encourage individuals to set goals as health benefits can be achieved from modest amounts of weight loss.
UK-wide problem
Obesity is on the rise throughout the whole of the UK, with even higher levels in England, Scotland and Northern Ireland than in Wales:
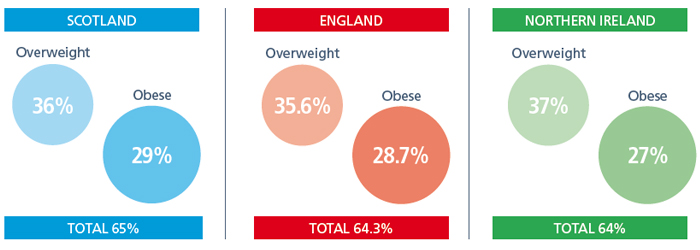
According to the latest House of Commons Library briefing paper on Obesity Statistics, it is difficult to directly compare Welsh obesity statistics with those in Scotland, England and Northern Ireland. Adult obesity is defined consistently across Scotland, England, Wales and Northern Ireland using the BMI scale. However, height and weight measurements are self-reported in Wales, whereas direct measurements are taken in the other three nations.
Encourage individuals to set goals as health benefits can be achieved from modest amounts of weight loss

active every day and limit their time
spent sedentary.
Alastair Buxton, director of NHS services at PSNC, says prevention is one of three key strands in the five-year Community Pharmacy Contractual Framework (CPCF) for England agreed by PSNC, the Department of Health and Social Care (DHSC) and NHS England and NHS Improvement (NHSE&I). “Helping to position pharmacies as healthy living centres, Level 1 Healthy Living Pharmacy (HLP) status has been part of recent quality schemes. By 1 April 2020, it will become an essential requirement for all community pharmacies. Accreditation as HLPs will transform the pharmacy network into hubs to promote health, wellbeing and self care,” he says. “The 2019/20 Pharmacy Quality Scheme’s prevention domain also encourages pharmacies to support key public health goals. Criteria include reducing the volume of sugar sweetened beverages sold by the pharmacy, meeting dementia-friendly environment standards and checking that people with diabetes have had annual foot and eye checks.”
A practical approach
When tackling weight management in a pharmacy setting, Tam Fry, chair of the National Obesity Forum, says that leaflets and other forms of information tend to be less effective than one-to-one conversations and that weight management discussions also need to be customer-led.
“People go into a pharmacy to buy medicines. They may bring up their weight in conversation at the counter, but it is a sensitive issue,” he says. “If customers are already taking medicine for a condition such as diabetes, a GP should already be discussing weight and lifestyle with them, but the pharmacy team could ask how things are going to see if they are getting enough support. Community pharmacies should have a room with a set of accurate weighing scales and a height measure, along with a colour-coded BMI chart showing underweight, normal, overweight and obese ranges. It is important to take BMI measurements over a period of time, such as two or three times over a few weeks or months, rather than as a on-off measurement, to see if the customer’s weight is changing.”
Ivo Vlaev, professor of behavioural science at Warwick Business School, has worked with PHE and the DHSC in developing health interventions. “Many people don’t want to talk about their weight, which can be a problem for healthcare professionals who want to help,” he says. “Group sessions often work very well, where people share an appointment and learn from each other. There’s also evidence that financial incentives work well for weight loss, so that people have a clear goal at the end, but this would need funding. There are very helpful apps out there that can encourage people to lose weight, eat healthily and exercise more, so this is something that pharmacies could recommend. Many of these apps feature virtual rewards, targets and goals.”
How much?
In September 2019, the chief medical officers in the UK issued updated physical activity guidelines. Recent evidence suggests that any amount of physical activity can be beneficial, even if it’s low intensity or low frequency, especially if people have low levels of physical fitness. The new guidelines include specific information for disabled adults and women during and after pregnancy.
To benefit health, physical activity should include a mixture of cardiovascular, muscle and bone strengthening and balance training.
- Under 1s: be physically active several times a day, including tummy time for those not yet mobile
- Toddlers (one to two years): have at least 180 minutes (three hours) of physical activity a day
- Pre-schoolers (three to four years): have at least 180 minutes (three hours) of physical activity a day, including at least 60 minutes of moderate-to-vigorous intensity physical activity
- Children and young people (five to 18 years): have moderate-to-vigorous intensity physical activity for an average of at least 60 minutes per day and limit sedentary time as much as possible
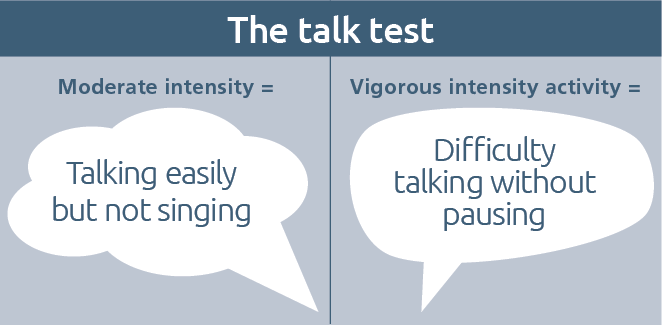
- Adults (19 to 64 years): should be physically active every day and reduce sedentary time. This means at least 150 minutes of moderate-intensity activity (e.g. brisk walking) each week, or 75 minutes of vigorous activity (e.g. running), or even shorter durations of very vigorous activity (e.g. sprinting or stair climbing), or a combination of moderate, vigorous and very vigorous activity. Muscle strengthening activities should be done on at least two days a week
- Disabled adults: should aim for at least 150 minutes each week of moderate intensity activity and strength and balance activities on at least two days per week
- Pregnant women: there is no evidence of harm to babies so pregnant women should aim for at least 150 minutes each week of moderate intensity activity and muscle strengthening activities on at least two days per week. They should listen to their body, adapt their activities as pregnancy progresses and avoid bumping the bump. The same is the case after birth, but increasing activity gently and including pelvic floor exercises
- Older adults (65+): at least 150 minutes of moderate intensity aerobic activity, building up gradually from current levels. Those who are already regularly active can achieve these benefits through 75 minutes of vigorous intensity activity, or a combination of moderate and vigorous activity, to achieve greater benefits. Weight-bearing activities help to maintain bone health.