Recognising endometriosis
In Population Health
Follow this topic
Bookmark
Record learning outcomes
Endometriosis is as common in women as diabetes, but diagnosis can take years, so helping spot the condition can make a huge difference to their lives
Endometriosis affects one in 10 women of reproductive age, which means there are around 1.5 million women in the UK currently living with the chronic and debilitating condition – the same number as diagnosed with diabetes.

Despite being so common the average diagnosis time is 7.5 years, leaving many women struggling to cope with the resulting painful or heavy periods and negative impact on their quality of life. In addition to the challenge of living with the pain of endometriosis, having a physical illness such as this significantly increases the chances of having poor mental health.
Devastating impact
A recent study conducted by the BBC has revealed the devastating impact that endometriosis has on women’s lives in the UK. Of the 13,500 women who took part:
- Nearly all said it had badly affected their career, sex life and mental health
- Most said it had impacted on their education
- Most said they rely on prescription painkillers every month, including potentially addictive opioids
- And around half said they had experienced suicidal thoughts.
“These figures are a stark reminder that physical and mental health are not felt separately”, says Sarah Hughes, chief executive of the Centre for Mental Health. “Health services need to wake up to the hidden and unspoken emotional pain too many women experience without the help they need to manage such a poorly understood and distressing condition.”
With this in mind, charity Endometriosis UK is calling on the Government to ensure that the NHS acknowledges the scale of endometriosis and plans services to support all those who need it, as well as investing in research to find the cause of the disease, better treatment and management options, and a cure.
The All-Party Parliamentary Group (APPG) for Endometriosis has committed to launching and overseeing an inquiry into endometriosis. Anna Turley MP, a member of the APPG for Endometriosis, says the data gave “millions of affected women a voice” and the APPG would be calling on the Government to act.
Pharmacy support
Pharmacy teams have a vital role in supporting and advising customers with endometriosis, as well as helping them receive a prompt diagnosis. But this means pharmacy staff need to be alert to signs of the symptoms (see panel overleaf).
This can be challenging because although period problems are very common, many women do not feel confident talking about them, either because they do not realise their experience is not normal, or because they are embarrassed to raise the issue.
“All too often, women are told their pain is ‘normal’ or ‘in their head’,” says Faye Farthing, campaigns manager at Endometriosis UK. “An understanding of endometriosis amongst pharmacy teams is vital as it means people with the condition receive the respect, dignity and knowledge that they deserve. Pharmacy teams could also promote and raise awareness of the symptoms of the condition in their [stores] so more people become aware of this condition that affects one in 10 women from puberty to menopause.”
If a customer thinks they may have endometriosis, the first step is for them to book an appointment with their GP. As the symptoms of endometriosis are also characteristic of other conditions, it is difficult to diagnose and so the more information they can provide to their doctor the better. For example, endometriosis usually causes cyclical problems and so advice from the Royal College of GPs is for women to record their pain levels and symptoms in a menstrual diary, which can be handwritten or templates can be found online or in an app.
Despite being so common the average diagnosis time is 7.5 years
Diagnosis and treatment
Scans, blood tests and internal examinations are not a conclusive way to diagnose endometriosis and a normal scan, blood test and internal examination does not mean that someone does not have endometriosis.
The only definitive way to diagnose endometriosis is by a laparoscopy. This is an operation in which a camera (a laparoscope) is inserted into the pelvis via a small cut near the navel. This allows the surgeon to see the pelvic organs and any endometrial implants and cysts. Occasionally, diagnosis is made during a laparotomy – a major operation, which involves opening the abdomen with a larger incision.
The good news is that there are ways of managing endometriosis and its symptoms. Types of treatment depend on the woman’s age, and whether she is trying to conceive, and include:
Surgery to alleviate pain by removing the endometriosis, dividing adhesions or removing cysts
Hormone treatment to block or reduce the production of oestrogen in the body. This means the endometriosis will be unable to continue growing and will help to relieve symptoms
Pain management.
While some people believe complementary therapies such as acupuncture, homeopathy and herbal medicine can help tackle endometriosis, there is a lack of evidence to recommend them. Signposting women to self-help groups can be useful to help sufferers improve their symptoms.
There are also some myths that exist about treatment that pharmacy staff can dispel for customers. For starters, pregnancy or hysterectomy is not a cure for endometriosis. In addition, as endometriosis affects women differently the treatment options that have worked for someone a customer knows may not necessarily be right for them. Similarly, just because they may have tried one option that didn’t work, it doesn’t mean something else won’t be a success. Finally, customers can be reassured that endometriosis is not caused by something they have done wrong – it is not an infection, it is not contagious, and it is not cancer.

The infertility link
There is an association between infertility and endometriosis but, according to charity Endometriosis UK, the cause has not been fully established.
Minimal to mild endometriosis is common and it is far more likely that women will have no difficulty conceiving naturally. With increasing severity of endometriosis, scar tissue (adhesions) becomes more common and the chance of natural conception decreases because scar tissue distorts the pelvic anatomy.
Endometriosis can cause delays in getting pregnant, but once a woman is pregnant, their pregnancy is expected to be no different from normal. In general, pain improves, but may return after giving birth as periods return.
Drug treatment for endometriosis does not improve fertility, either during or after treatment. It is only indicated for treatment of pain associated with endometriosis or as a preparation for surgery. However, surgical treatment of the condition improves fertility and helps pain. The aim of surgical treatment is to destroy or cut out (excise) endometriotic nodules and release adhesions. However, even with severe endometriosis, natural conception is still possible.
According to research from Endometriosis UK:
- If 100 women without endometriosis all start trying for a baby, at the end of one year, 84 will be pregnant
- If 100 women with minimal-mild endometriosis all start trying for a baby, at the end of one year, 75 will be pregnant
- If 100 women with moderate endometriosis all start trying for a baby, at the end of one year, 50 will be pregnant
- And if 100 women with severe endometriosis all start trying for a baby, at the end of one year, 25 will be pregnant.
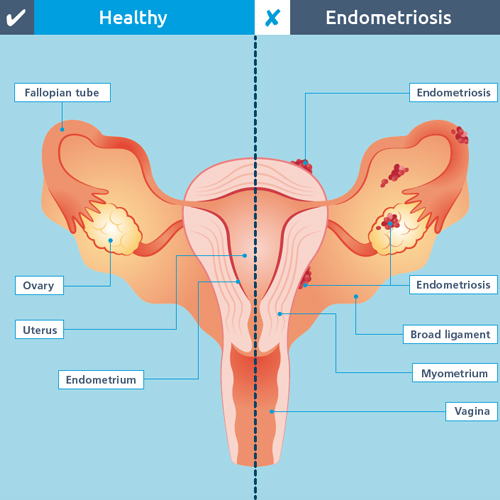
Endometriosis explained
Endometriosis is a chronic and debilitating condition that causes painful or heavy periods and may also lead to infertility, fatigue, and bowel and bladder problems. It can affect all women and girls of a childbearing age, regardless of race or ethnicity, and research has yet to find a proven cause.
What it is
Every month a woman’s body releases hormones, which cause the lining of the womb to thicken in preparation for a fertilised egg. If pregnancy does not occur, this lining will break down and is released from the body as a period.
Endometriosis cells react in the same way – except that they are located outside the womb. During the monthly cycle hormones stimulate the endometriosis, causing it to grow, then break down and bleed. This internal bleeding, unlike a period, has no way of leaving the body. This leads to inflammation, pain, and the formation of scar tissue, known as adhesions.
Endometriosis is most commonly found inside the pelvis, around the ovaries, the fallopian tubes, on the outside of the womb or the ligaments that hold the womb in place, or the area between the rectum and womb called the pouch of Douglas. It can also be found in the ovaries, on the bowel, bladder, intestines, vagina and rectum. Endometrial tissue can also grow in the muscle layer of the wall of the womb, which is a condition called adenomyosis – see opposite.
Symptoms
The classic symptoms of endometriosis are:
- Painful periods
- Painful sex
- Infertility.
Women with the condition also report other symptoms, including:
- Pain starting before periods
- Ovulation pain
- Pre-menstrual spotting
- Loss of dark or old blood before a period or at the end of a period
- Leg and back pain
- Heavy periods with or without clots
- Prolonged bleeding and irregular periods
- Painful bowel movements
- Pain when passing urine
- Pain on internal examination
- Lethargy and extreme tiredness
- Nausea
- Depression.
The majority of women with endometriosis will experience some of these symptoms. Some women with the condition will have no symptoms at all, and the amount of endometriosis does not always correspond to the amount of pain.
Identifying adenomyosis
Painful or heavy periods can also be a sign of a condition called adenomyosis, where endometrial tissue grows inside the muscle wall of the womb (myometrium) and responds to the hormonal changes each month, causing severe pain.
Around one in 10 women with endometriosis will have adenomyosis. It can occur in any woman who still has periods, but is most common in those aged 40-50 and in women who have had children. The most common symptoms are heavy, painful or irregular periods, and pre-menstrual pelvic pain and feelings of heaviness and/or discomfort in the pelvis. Less common are pain during sexual intercourse or pain related to bowel movements.
In at least half of cases, adenomyosis can be detected by an internal transvaginal ultrasound scan, but if that does not clearly show adenomyosis it may be necessary to have an MRI scan.
Treatment options for adenomyosis include:
- Doing nothing – if symptoms are mild; the woman is trying for a baby; or is nearing menopause, when symptoms tend to stop, treatment may not be necessary
- Non-hormonal medicines (for example, tranexamic acid and mefenamic acid) to help reduce pain and bleeding
- Hormonal medicines, which can include the combined oral contraceptive pill; progestogen-only pill; or the intrauterine system (IUS), also known as the hormonal coil
- Injections of hormones to cause a temporary and reversible menopause
- Hysterectomy for women who do not want to become pregnant
- Uterine artery embolisation, which is where tiny particles are injected into blood vessels through a catheter in the groin to cut off the blood supply to the adenomyosis. This is less invasive than surgery and may help preserve fertility.
Adenomyosis does not seem to decrease the chance of getting pregnant, but it may increase the risk of miscarriage or having a premature baby. It is important to reassure women that if adenomyosis occurs it is not because they have done anything wrong, and that it is not cancerous and cannot be spread between people.
Yoga, meditation and gentle exercise may help with painful periods, but women should always talk to their GP and ask for further help.
Unfortunately, with both endometriosis and adenomyosis some women will have difficulty finding a resolution that works for them. As ever, the role of the pharmacy team is to give them the most accurate advice and the best support possible as they continue on their journey towards diagnosis and treatment.
Further information
- Endometriosis UK – Understanding Endometriosis Information Pack
- Royal College of GPs’ Menstrual Wellbeing Toolkit, developed in partnership with Endometriosis UK, is an easy-to-use, logical, evidence-based resource for GPs and other primary care clinicians to help diagnose, support and manage problems caused by menstrual dysfunction
- Adenomyosis Advice Association
- Guy’s and St Thomas’ NHS Foundation Trust – adenomyosis patient leaflet.
