The enigmatic aura
In Clinical
Follow this topic
Bookmark
Record learning outcomes
Could you tell the difference between a migraine aura and a transient ischaemic attack or stroke?

“I was terrified,” admits 56-year-old Jack. “I saw a flashing light in the corner of my right eye. This developed into a shimmering, colourless, bright, irregular zig-zag that fragmented and distorted my vision as it wobbled across my sight. After a few minutes, I couldn’t see the computer screen. Gradually, the distortion faded.
“The first time it happened, I was really worried. I thought I was having a stroke. I’ve experienced it several times now and I know it’s a migraine aura, but I’ve never had the headache.”
Auras occur during or before at least a third of migraines.1 In about a fifth of migraines with aura, headaches start before or with the aura1 but only 19 per cent of people who experience migraine with aura experience the visual and other symptoms every time.2 As with Jack, people can experience migraine aura without ever developing headaches, which can cause confusion with diagnosis.3
Auras vary widely between people and in the same person over time. Apart from lights and blurred vision, migraine auras can cause Lilliputian or Brobdingnian hallucinations (where objects seem too small or too large), misperceptions of distance and tunnel vision.1
Occasionally, patients experience olfactory hallucinations. A 53-year-old woman, for example, reported smelling a “dirty dog” as part of her aura, which, usually, did not develop into a migraine. The smell could occur up to two or three times a day and last for up to an hour.4
Origins of auras
Auras seem to arise from a wave of electrical depolarisation that spreads through the neurones and glial cells, which support and protect nerve cells, in the cortex (grey matter).1,5 This ‘cortical spreading depression’ (CSD) affects many parts of the brain causing, for example, visual symptoms, muscle weakness, sensory problems such as paraesthesia and language disturbances.1 Auras typically develop over at least five minutes and can last for up to an hour.1
“Attacks of migraine aura without subsequent development of headache become relatively common as people with a history of migraine with aura become older,” says Susan Haydon, support services manager at the Migraine Trust.
Why refer?
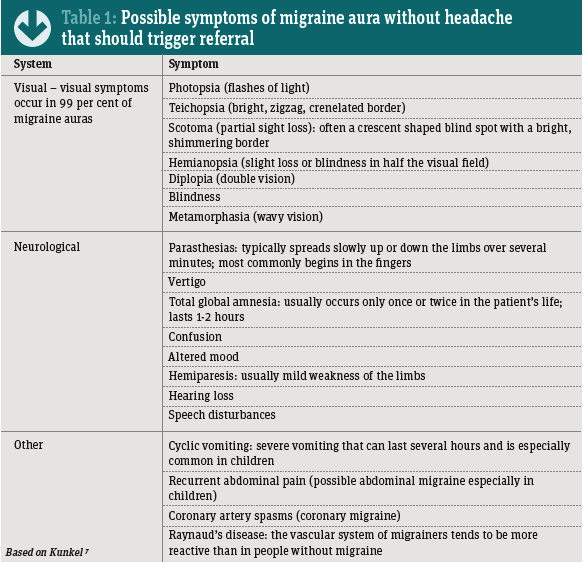
Aura without headache is benign6 but pharmacists should immediately refer people who report symptoms (see Table 1) to exclude, for example, transient ischaemic attacks (TIA), stroke and epilepsy.6
Certain clinical clues help differentiate the possible competing diagnoses. For instance, the evolving CSD means that the visual changes in aura without headache tend to be dynamic and often colourful, bright and shimmering. Visual changes in TIA tend to be a static loss of vision over half the visual field. TIAs tend to last about three to 10 minutes rather than the 15-30 minutes characteristic of a migraine aura.6,7
Some people who experience recurrent vertigo despite normal auditory and vestibular testing have migraine aura without headache.7 Retinal disease – such as detachment, which is a medical emergency – can cause flashes of light but these tend to be more persistent than in aura without headache.7 Recurrent visual symptoms that last for more than an hour may indicate, for example, retinal disease, recurrent emboli, coagulopathy or vasculitis.7
Parasthesias in aura typically spreads up or down the limbs over several minutes, usually starting in the fingers. In partial epileptic seizures, the numbness and tingling spreads through the limb in a few seconds.7 Visual disturbances in partial seizures also typically last less than five minutes.7 None of these are diagnostically definitive and patients should be referred.
As aura without headache is benign,6 patients generally need only reassurance once the other possible causes are ruled out. Community pharmacists can signpost patients to the Migraine Trust (see panel) and could suggest sufferers keep a diary to see if they can identify any triggers, such as stress at work or home, certain foods and drinks or changes in sleep patterns.
“There are no acute treatments for attacks of migraine aura without headache,” Susan Haydon concludes. “Management of migraine aura without headache is generally preventive. This may include lifestyle adjustments to avoid personal migraine trigger factors and building routine into daily life – the migrainous brain does not like change.
“If attacks are frequent and impact on quality of life, a course of preventive medicine is required to reduce frequency and severity of migraine. If the doctor is not sure of the diagnosis, they may refer for scans or to a headache clinic. It is critical that community pharmacists refer people with aura, whether or not they develop headaches, to their GP as soon as possible.”
Further information
The Migraine Trust offers an information service and an advocacy service to help people understand, manage and live with migraine.
Tel: 0203 9510 150 Website: migrainetrust.org
